Pega Foundation for Healthcare company / group contract record
Pega Foundation for Healthcare
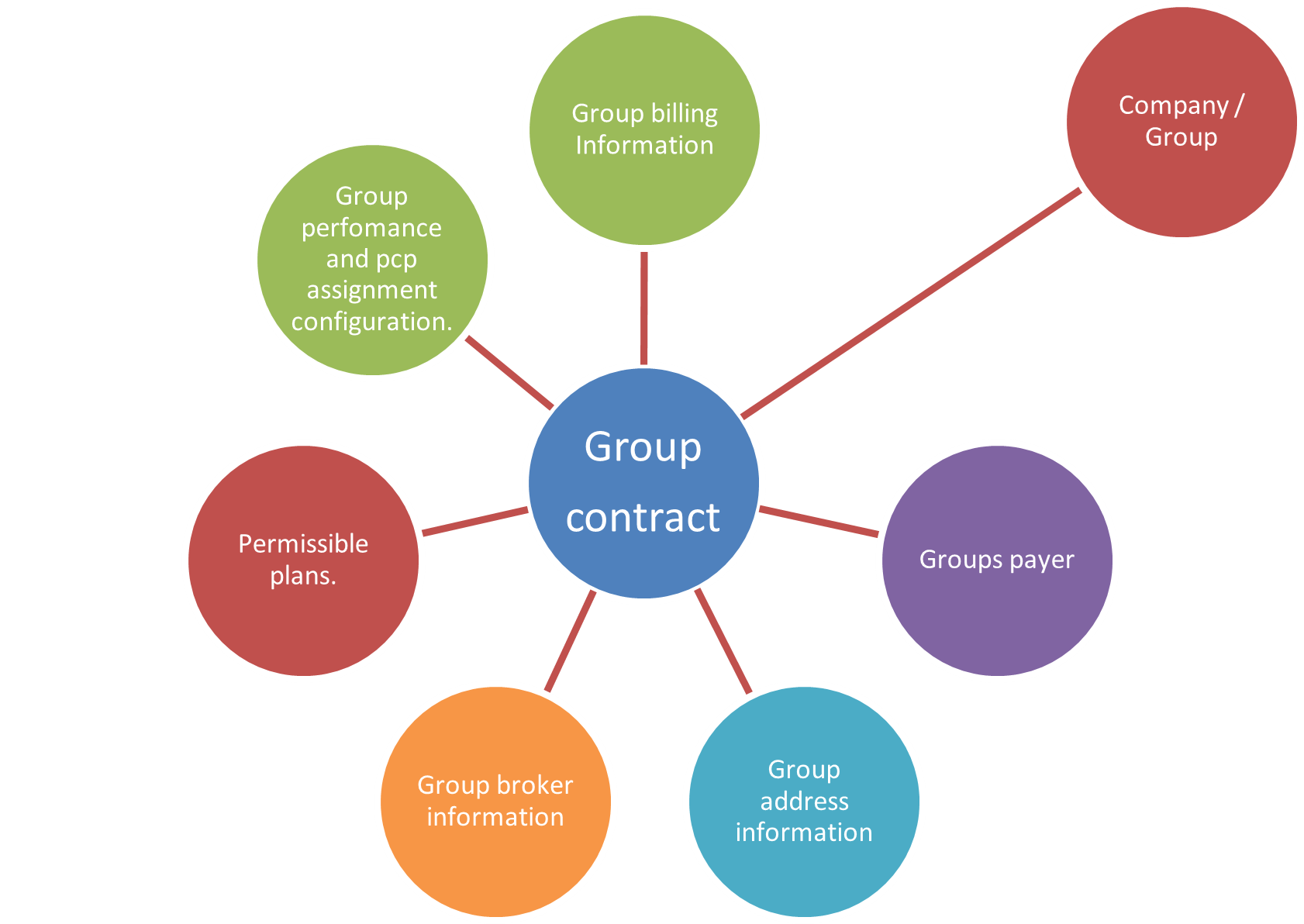
Group contract definition: A group contract can be defined as an entity created to configure rules and capture details about a healthcare company / group. A group contract is used to:
- Capture additional details about the group. (billing information, broker information, and so on.)
- Help manage the rules around enrolling members in a group. The contract houses
configurations which validate:
- Member’s enrollment period.
- Member’s PCP.
- Member’s plan within the group.
Previous topic Company class structure Next topic Manually creating a group contract record
