Complaint - Use-case (UC) 1: Create complaint
This functionality performs a search of selected code sets type using specific search criteria (as code only) and displays the results.
To create a complaint, complete the following steps:
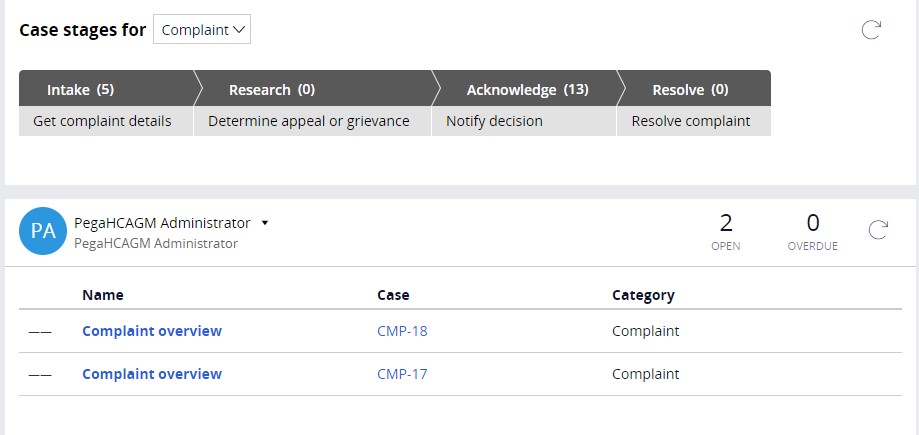
- Log in to the Appeals and Grievance (A&G) User Portal using administrator
credentials. The system displays the user dashboard with all cases assigned to
the user.
- Click New on dashboard and click New Complaint to create a new complaint.
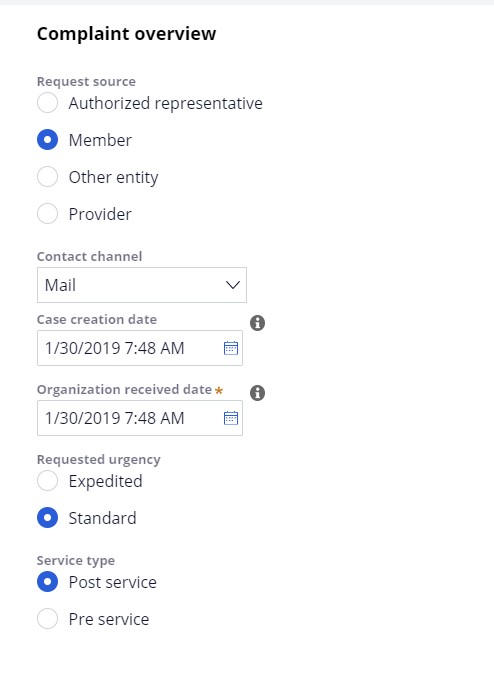
- Select Member as the Request source from the following
options:
- Authorized Representative
- Member
- Other Entity
- Provider
- Select the appropriate Contact Channel from the following options:
- Broker
- Compliance Line
- CTM (Complaints tracking module)
- DOI (Department of Insurance)
- Fax
- Phone
- Social Media
- Web Self-Service
- Enter or select a date on which the case is created.
- Enter or select a date on which the case was received by the organization.
- Select the Urgency and Service Type.
- Click Continue at the bottom right of screen.
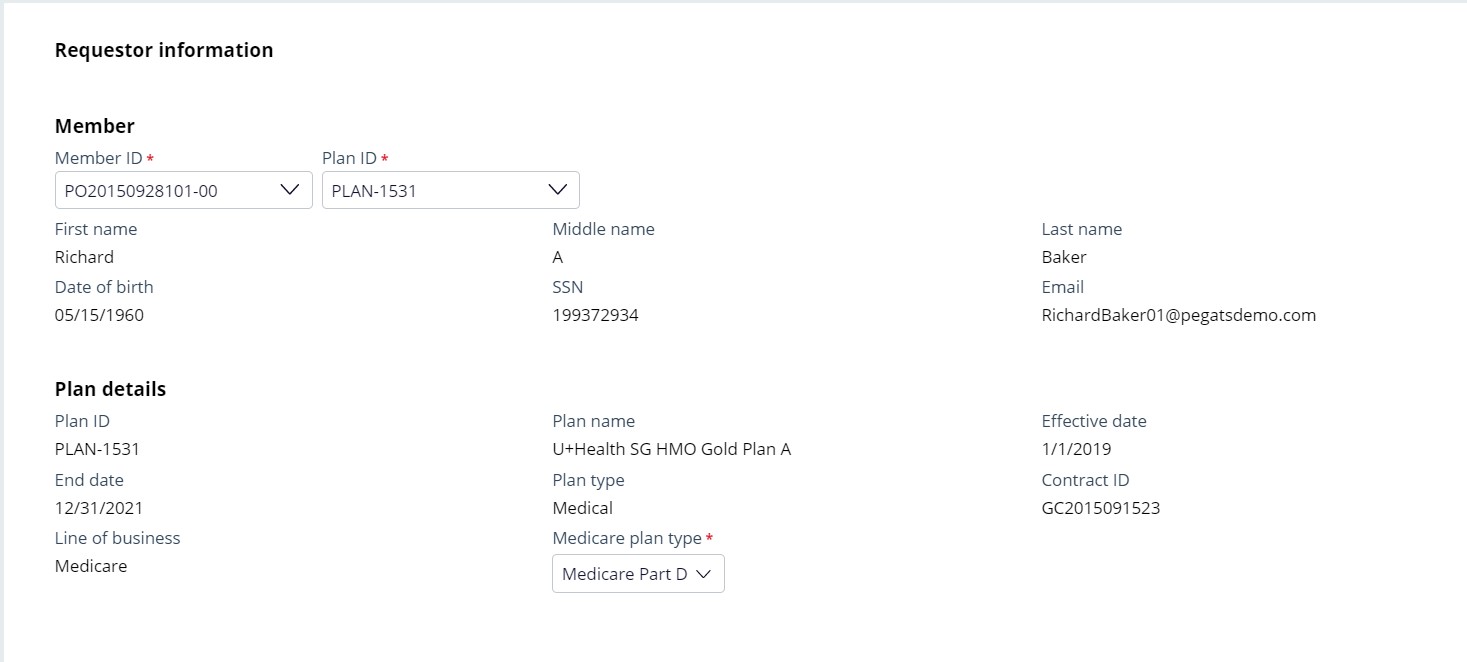
- Select Member ID to auto-populate member information. The system allows user to search by selecting a member from the drop-down, or by entering Member ID number, first name, or last name. Note the system only allows selection of a single member record.
- Select Plan ID. The system only allows selecting one of the plans in the
system.
The system displays the following plan details:
- Plan ID
- Plan Name
- Effective Date
- End Date
- Plan Type
- Contract ID
- Line of Business
Medicare plan type (displayed when member’s Plan ID Line of Business is Medicare)
- Verify Member details and then click Continue.
- Click Add reason to add category of complaint and the
reason for complaint.
System displays following four categories and associated reasons:
- Health Plan
- Payment/Copayment
- Provider
- Treatment Procedure
- Prescription Drug
- Select one of the Complaint categories and one associated reason.
- If the complaint category is Health Plan, the system gives option to capture Contact Name, Contact Phone, and Incident Date.
- If the complaint category is Treatment procedure, the system gives option to capture Submission type, Type of Service, Place of Service, Service Date, Name of Service Provider, Type of Service Provider, and Prior Authorization Number. Based on the value selected for submission type, system gives option to capture either Claim ID or Authorization ID.
- If the complaint category is Provider, the system gives option to capture Contact Name, Contact Phone, and Incident Date.
- If complaint category is Payment/Copayment and the complaint
reason is one of the following, the system gives option to capture Claim
ID and Authorization ID:
- Discontinued Service
- Plan Responsibility
- Should be a covered service and plan Responsibility (this is single complaint reason)
If the Medicare plan type is Medicare Part D and complaint category is Prescription drug, for any selected complaint reason the system gives option to capture Claim ID or Authorization ID based on the ‘Submission type’ value selected and also an option to capture whether the member is residing in long term care facility and prescribing provider’s information.
- Enter comments in Complaint justification to capture more details about
complaint.
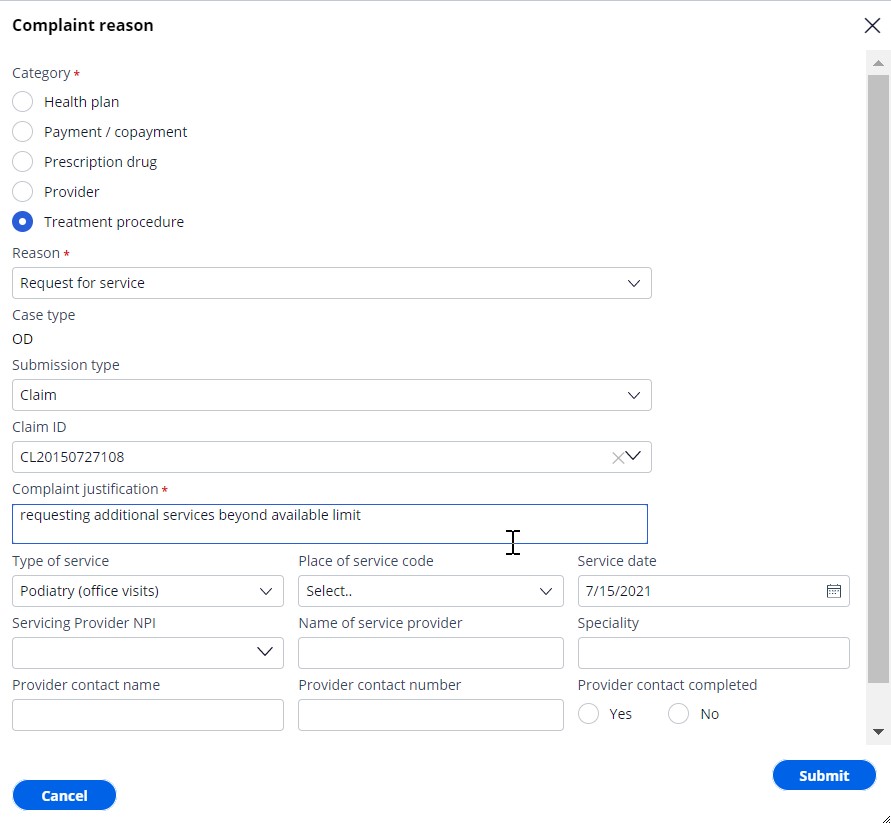
- System indicates child case type based on complaint category and reason. Possible child case types are: Appeals, Grievance and Organization Determination (OD).
- System provides an option to capture Good cause reason to articulate why a complaint that has been filed outside of the allowable limit is being considered.
- Click Submit to create child cases and forward the complaint for processing further.
- If required, click Add Reason to add more than one
complaint. Repeat steps 11 to 17.

- Click Submit at the right bottom of Complaint screen.
The system generates an appeal, determination, or a grievance subcase based on Complaint
Category and Complaint reason as per table below:Complaint category Complaint reason Appeal or grievance Payment/Copayment General dissatisfaction Grievance Amount different than last year Grievance Change in premium Grievance Plan responsibility Appeal Type of service not correct or not at right level Appeal Discontinued Service Appeal Timing of plan payment Appeal Should be a covered service and plan responsibility Appeal Treatment/Procedure Notification of termination of service Appeal Notification of denial of service Appeal Reduction of previously approved service Appeal Refusal to authorize service Appeal Request for payment OD (Determination) Request for service OD(Determination) Provider Current provider no longer contracted Appeal Timeliness of service Grievance Quality of Service Grievance Health Plan Rudeness / disrespect by staff Grievance Enrolment / disenrollment issue Grievance Plan Benefit issue Grievance Pharmacy access issue Grievance Customer service issue Grievance CMS issue Grievance Other issues Grievance Process issues Grievance Marketing issues Grievance Prescription drug Request Non-Formulary Exception - Drug not on plan OD (Determination) Request Non-Formulary Exception - Drug no longer offered on
plan OD (Determination) Request Formulary Exception - Step therapy exception OD (Determination) Request Formulary Exception - Request higher dosage or quantity
than limit OD (Determination) Request Tiering Exception - Drug in higher cost-share
tier OD (Determination) Request Tiering Exception - Drug moved to higher cost-share
tier OD (Determination) Request prior authorization for prescribed drug OD (Determination) Request out-of-pocket expense reimbursement for covered
drug OD (Determination) Charged copay higher than plan limit for a drug OD (Determination)
Previous topic Business overview Next topic Complaint - UC 2: Hold case for missing AOR
