Assigning member penalties
The financial liability associated with violating a payer’s billing policies and procedures often falls on the healthcare provider, as in the case of a physician who bears the cost of a denied claim resulting from the submission of incorrect or incomplete information. Members may also bear financial liability under certain circumstances, most commonly around service authorizations. For example, a member may be penalized for failing to obtain an authorization in a timely manner. But financial liability isn’t limited exclusively to claim costs; in fact, members and providers may incur penalties above and beyond the cost of the service itself.
SCE’s approach to determining and applying member penalties during the claims adjudication process includes:
- Leveraging SCE’s auth processing logic to accommodate the selection and application of auth and penalty variations configured in an external benefit system (e.g., PCS),
- using decision tables and action codes to drive penalty calculation and claims pricing logic, and
- executing work flows that cross-walk penalty variations to action codes, and action codes to penalty calculations.
The following graphic represents the end-to-end process for identifying and processing penalties within SCE’s CE_ProcessAuthorization module.
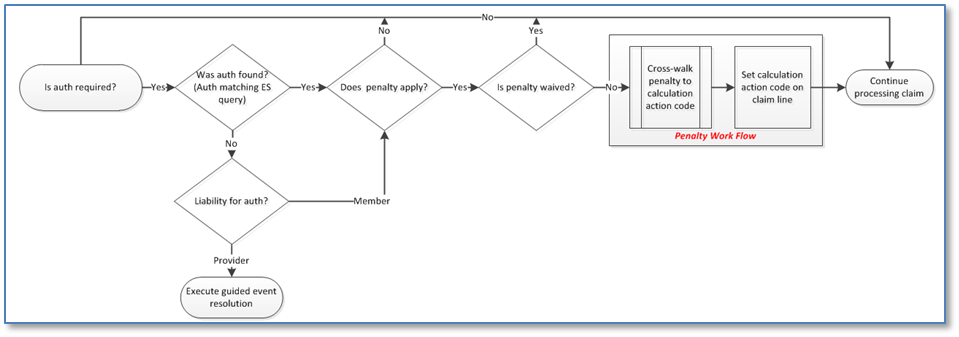
During the execution of the CE_ProcessAuthorization module, SCE determines whether an authorization is required for the claim/line being adjudicated. If no auth is required, the remaining steps in the auth process are bypassed. If required, SCE then executes the auth matching ES query.
Depending on the results of the ES query:
- If no matching auth is found, SCE then determines whether the member or the provider is liable for that auth. If the provider is liable, SCE follows the current guided event resolution path for no authorization found. However, if the member is liable, SCE triggers an action code (PA-101) to bypass the guided event resolution process, and then determines whether a penalty applies. If no penalty applies, the claim/line proceeds along the normal adjudication path. However, if a penalty applies, SCE next determines whether the penalty will be waived. If it is waived, the claim/line proceeds along the normal adjudication path. If it is not waived, the claim/line is sent to the penalty work flow.
- If a matching auth is found, SCE then determines whether a penalty applies. If no penalty applies, the claim/line proceeds along the normal adjudication path. However, if a penalty applies, SCE then determines whether the penalty will be waived. If it is waived, the claim/line proceeds along the normal adjudication path. If it is not waived, the claim/line proceeds to the penalty work flow.
Previous topic Authorization processing work flow Next topic Penalty work flow
