Step 1 - Member information
This step lets you enter patient and subscriber information, as well as other insurance payment information, if required.
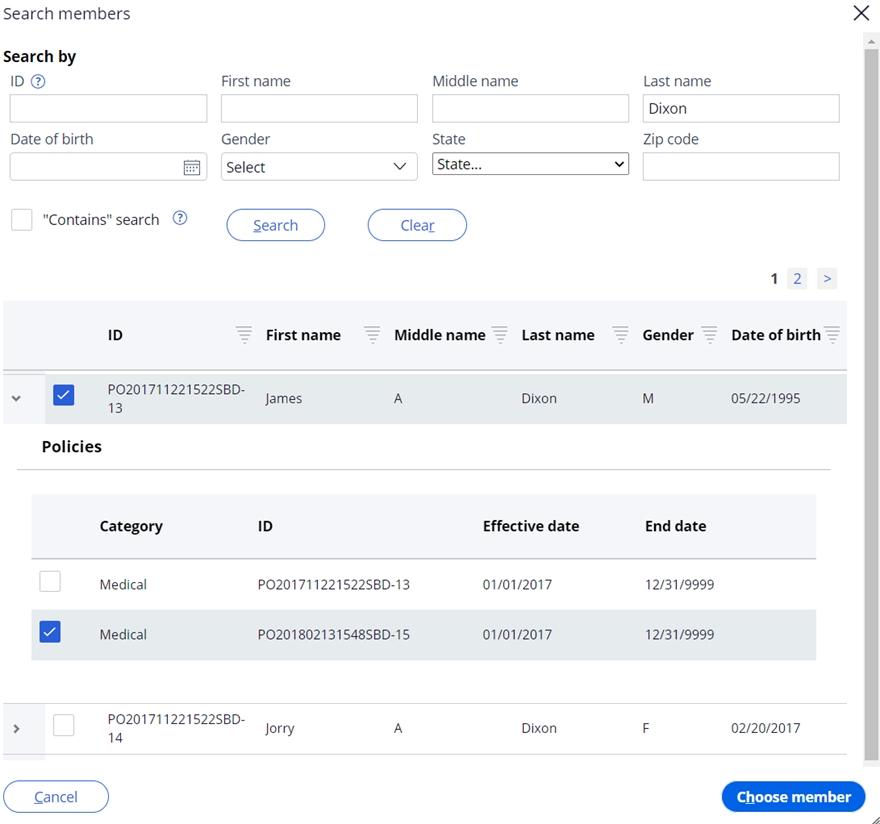
SCE provides the option for you to search for and select a member during manual claim entry. Open the search by clicking Search members at the bottom right of the member information slot. A modal with search fields opens. Selecting a member returned in the search and clicking Choose member auto populates the Patient ID field and other demographic fields on the screen, assuming the data is available in the member system.
Senior claims examiners also have the option to manually choose a policy – but this policy will be used only to populate the patient ID in the patient section in order to proceed further with claim entry. The actual policy selection for the claim occurs in the policy selection and eligibility module.
The fields in the member information step are listed below and are displayed when entering professional, institutional, and dental claims. The * indicates a required field.
| Step/Section | Field | Definition |
| Member information | Patient ID | The patient’s identification number. If the ID is matched to an existing member record, other demographic fields on the screen will auto populate, assuming the data is available in the member system. |
| Member information | Policy role/relationship* | The patient’s relationship to the subscriber. Select from the drop-down list. |
| Member information – PERSONAL INFO | First name | First name of the patient |
| Member information – PERSONAL INFO | Middle | Middle name or initial of the patient |
| Member information – PERSONAL INFO | Last name* | Last name of the patient |
| Member information – PERSONAL INFO | Gender* | Gender of the patient. Select from the dropdown list. |
| Member information – PERSONAL INFO | Date of birth* | Date of birth of the patient. Use the date picker or enter as MM/DD/YYYY |
| Member information – PERSONAL INFO | Address 1* | The first line of the patient’s address |
| Member information – PERSONAL INFO | Address 2 | The second line of the patient’s address |
| Member information – PERSONAL INFO | City* | The patient’s city |
| Member information – PERSONAL INFO | State | The patient’s state. Choose from the dropdown list. |
| Member information – PERSONAL INFO | Zip | The patient’s zip code |
| Member information – PERSONAL INFO | Phone | The phone number of the patient |
| Member information – PERSONAL INFO | The email address of the patient | |
| Member information – POLICY | Subscriber | The policy subscriber’s first and last name followed by their ID |
| Member information – POLICY | Payer Responsibility sequence number code* | Indicates the policy’s order of responsibility for adjudicating the claim. Choose from the dropdown list. |
| Member information – POLICY | Plan name | The plan name |
If subscriber data changes are required, select the gear icon next to the policy number to open a modal and update subscriber demographic information. The fields available in the modal are listed below and are displayed when entering professional, institutional, and dental claims.
| Step/Section | Field | Definition |
| Update subscriber details | Subscriber ID* | The ID of the subscriber |
| Update subscriber details | Policy role/relationship | The relationship code of the subscriber. Note that this is set to 00 – Subscriber and cannot be updated. |
| Update subscriber details | Payer name | The payer name for the policy |
| Update subscriber details – PERSONAL INFO | Full name* | The first, middle, and last name of the subscriber |
| Update subscriber details – PERSONAL INFO | Gender | The subscriber’s gender. Select from the dropdown list. |
| Update subscriber details – PERSONAL INFO | Date of birth | Date of birth of the subscriber. Use the date picker or enter as MM/DD/YYYY |
| Update subscriber details – PERSONAL INFO | Address line 1 | The first line of the subscriber’s address |
| Update subscriber details – PERSONAL INFO | Address line 2 | The second line of the subscriber’s address |
| Update subscriber details – PERSONAL INFO | City* | The subscriber’s city |
| Update subscriber details – PERSONAL INFO | State | The subscriber’s state. Choose from the dropdown list. |
| Update subscriber details – PERSONAL INFO | Zip | The subscriber’s zip code |
| Update subscriber details – PERSONAL INFO | Phone | The phone number of the subscriber |
| Update subscriber details – PERSONAL INFO | The email address of the subscriber |
The lower right side of the Member information slot displays the Patient has other policies (COB) checkbox. Selecting the check box allows you to + Add other policies for coordination of benefits purposes. The fields in the Add other policy subscriber modal are listed below and are displayed when entering professional, institutional, and dental claims.
| Step/Section | Field | Definition |
| Add other policy subscriber – OTHER SUBSCRIBER | Other subscriber ID* | The other policy subscriber’s ID number |
| Add other policy subscriber – OTHER SUBSCRIBER | Individual relationship code* | The relationship code of the patient to the other subscriber |
| Add other policy subscriber – OTHER SUBSCRIBER | Payer Responsibility sequence number* | Indicates the policy’s order of responsibility for adjudicating the claim. Choose from the dropdown list. |
| Add other policy subscriber – OTHER SUBSCRIBER | Last name | The last name of the other subscriber |
| Add other policy subscriber – OTHER SUBSCRIBER | Benefit assignment indicator* | Choose from Yes, No, or Not applicable |
| Add other policy subscriber – OTHER SUBSCRIBER | First name | The first name of the other subscriber |
| Add other policy subscriber – OTHER SUBSCRIBER | Release of information* | Choose I or Y |
| Add other policy subscriber – OTHER PAYER | Other payer ID* | The plan ID of the other payer |
| Add other policy subscriber – OTHER PAYER | Payer name* | Name of other payer |
| Add other policy subscriber – OTHER PAYER | Claim control number | Other payer claim number |
| Add other policy subscriber – OTHER PAYER PAYMENT | Paid amount | Amount paid by the other payer |
| Add other policy subscriber – OTHER PAYER PAYMENT | Check number | The check number of the other payer’s claim payment |
| Add other policy subscriber – OTHER PAYER PAYMENT | Patient’s remaining liability | Patient liability from the other payer |
| Add other policy subscriber – OTHER PAYER PAYMENT | Paid date | The paid date of the other payer’s claim payment |
| Add other policy subscriber – OTHER PAYER PAYMENT | Non covered amount | Amount not covered by the other payer |
The lower right side of the Add other policy subscriber provides an area to enter claim level adjustments. Clicking + Add adjustment group code provides access to enter information in the fields listed below and are displayed when entering professional, institutional, and dental claims.
| Step/Section | Field | Definition |
| Add other policy subscriber – CLAIM LEVEL ADJUSTMENTS | Adjustment group code* | The claim adjustment group code; choose from the dropdown list. |
| Add other policy subscriber – CLAIM LEVEL ADJUSTMENTS | Reason code* | The claim adjustment reason code; choose from the dropdown list. |
| Add other policy subscriber – CLAIM LEVEL ADJUSTMENTS | Amount* | Amount adjusted by the other payer |
| Add other policy subscriber – CLAIM LEVEL ADJUSTMENTS | Quantity | The service units adjusted by the other payer |
Notes:
- You may enter multiple Reason codes, Amounts, and Quantities under a single Adjustment group code by clicking +Add reason code
- You may enter multiple adjustment group codes (and associated information) by clicking +Add adjustment group code
Once you have entered the member information, click Next on the bottom right of the screen to advance to the next step.
Previous topic Manual claim entry Next topic Step 2 - Providers
