Appeal
An appeal is a request for your health insurance company, the health insurance payers from the provider, or the patient to review a decision that denied an authorization.
To create an appeal case, in the Patient 360 profile of a specified member, click .
For more information about appeal case management, see the Pega Care Management Business Use Case Guide.
The following list describes items that are related to the Appeal Microjourney:
- Data model
- Rules for the list of sources in the appeal intake
- Updating the number of expiration days based on category code
- Updating the status based on the decision
- Determine resolution correspondence template
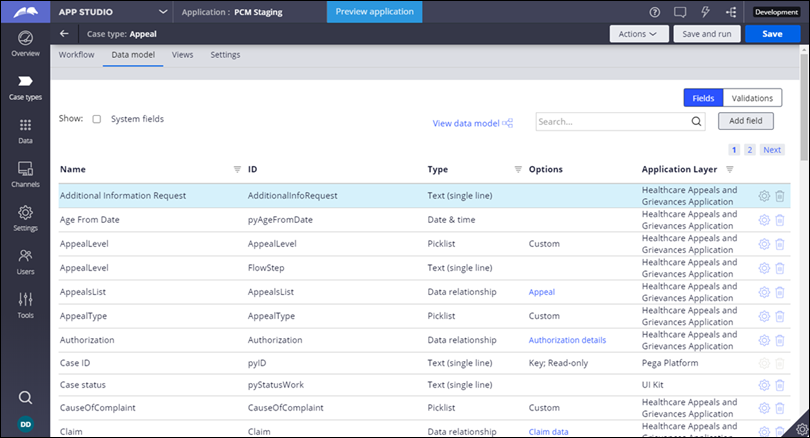
Data model
In App Studio, you can view the data model for Appeal in Case types.
Click the Data model tab on the Appeal page.
Rules for the list of sources in the appeal intake
To create an appeal case in the Pega Care Management application, fill in the required details such as contact channel, urgency, requesting provider, member, and denied authorization list. Use the following rules to configure a different source based on your organization's requirements.
Key rules for the list of sources
| Step in the intake and rule name | Rule type | Purpose |
| Metadata pyContactChannel | Property - Field value | Source for the Contact channel drop-down list (CL:PegaHC-AGWork) |
| Metadata Urgency | Property - Field value | Source for the Urgency drop-down list (CL:PegaHC-AG-Work) |
| Select requesting provider
D_GetProviderList | Data page | Searches for the requesting or service provider |
| Select
Member D_MemberPresentFuturePol | Data page | Searches for member policies. Member ID is the parameter. |
| Select prior Auth
request D_ListOfDeniedAuthorizations | Data page | Searches for denied authorizations from which you can choose for the appeal case. Member ID is the parameter. |
FinalDisposition | Property - Prompt list | Source for the Final disposition drop-down list. If you choose Uphold, then the Approved days, Status, and Reject reason fields are read-only. If you choose Overturn, you can edit the fields. |
Updating the number of expiration days based on category code
After the intake is complete, appeals are routed to medical directors for review. During the review, if the appeal is approved, then the system captures CertificationIssueDate and CertificationEffectiveDate as system dates and CertificationExpirationDate based on the authorization type, for example inpatient or outpatient.
Use this decision tree rule to make updates to the expiration days based on the request type.
Rule for expiration days
| Rule name | Rule type | Purpose |
| SetExpirationDays | Decision tree | Sets the number of expiration days based on the category code |
Updating the status based on the decision
Based on the decision outcome, the status of the authorization is set. You can update the status of the authorization based on the authorization decision and the reject reason that you configured. For example, you could change Reject to Denied.
Rule for updating the resolution status
| Rule name | Rule type | Purpose |
| ResolutionStatus | Decision table | Evaluates the resolution decision based on the authorization decision and the reject reason, if applied |
Determine resolution correspondence template
Based on the appeal decision outcome, correspondence is sent to the respective parties. You determine the correspondence template by using a decision table.
Use the ResolutionCorr decision table.
Previous topic Discharge Planning Next topic Authorization Request
