Concurrent Review
A concurrent review is a method of reviewing patient care and services during a hospital stay to validate the necessity of care and explore alternatives to inpatient care. It is also a form of utilization review that tracks the consumption of resources and the progress of patients while being treated.
By using the concurrent review, you can determine if the services that are being covered or provided are determined to be medically necessary and should continue to be covered. Industry guidelines such as Change Health's InterQual or MCG’s CareWebQi are used to create consistent, evidence-based decisioning.
The concurrent review case is a child case of the admission case. This case is automatically added as a child case of the admission case for certain diagnosis and procedure codes and also is based on the length of stay. The implementation layer can configure these values.
If the admission case requires a concurrent review, the discharge worksheet is not initially added under the discharge plan in the admission case tree. The system adds the discharge worksheet at the time of completion of the concurrent reviews. Otherwise, if the admission case does not require a concurrent review at this point, the discharge worksheet is directly added to the discharge plan in the admission case tree and provides you with the option to add a concurrent review on an ad-hoc basis.
If nurses determine that the progression criteria, used to determine if additional coverage should be provided, is not met, then you need to complete these fields:
- Authorized from date
- Authorized To Date
- Days denied
- Denial reason
For more information about concurrent reviews, see the Pega Care Management Business Use Case Guide.
The following list describes items that are related to the Concurrent Review Microjourney:
- Data Model for Concurrent review
- Key rules
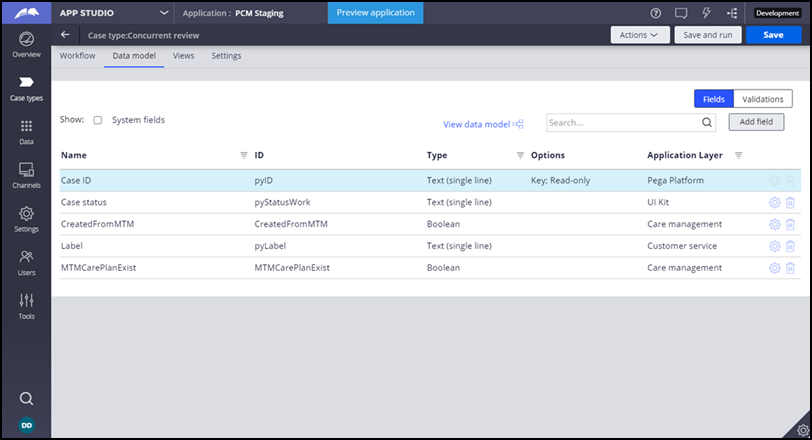
Data model
In App Studio, you can view the data model for Concurrent Review in Case types.
Click the Data model tab.
Key rules
While working on a concurrent review, nurses can access information such as level of care and diagnosis codes that were captured in the admission case. You can customize the rules in the following table to meet your organization's needs.
Key properties
| Rule name | Rule type | Purpose |
| SuggestedLOC | Property - Local list | Source for the Current LOC drop-down list |
| IsProgressionMet | Property - Local list | Source for the Progression criteria met
drop-down list. If nurses determine that the progression criteria, which
is the criteria that is used to determine if additional coverage should
be provided, is not met, then you need to complete these fields:
|
Use the D_fetchCategories data page with the DenialReason field as the source for the Denial Reason list. The ReviewDetails page list contains all past review details for the admission case.
When updating a case, the note that indicates the reason for the update is saved in the Conversation logs In the patient profile with the SaveConversation activity.
Previous topic Admission Next topic Discharge Planning
