Definition of Pega Care Management application components
With the reusable components that are described in this topic, you can create and maintain care plans to manage programs that are based on the needs and designs to meet your business objectives. Your care management application provides a guided process to help you define components that are needed for care plans, programs, and the personal health plan.
The dashboard in the Business Analyst portal provides a system administrator or a business analyst access to instances of configured rules such as goals, tasks, interventions, and alerts for the management of chronic conditions and wellness and preventative programs. Each rule type has its own template for creating and maintaining these instances. At run time, when these rules are called in the context of a patient’s care plan, a work object is created. With these reusable components, you can create and maintain care plans to manage programs that are based on the needs and designs to meet your business objectives.
You must plan for and create the instances of the following rule types to meet your business needs:
- Program category
- Specifies the name of the clinical category in which the program is being managed, such as Care Management, Disease Management, and Health and Wellness.
- Program
- Specifies the name of the clinical condition or chronic disease program that is being managed such as Diabetes, Asthma, Smoking Cessation, Post-Discharge or Re-Admission Prevention, Falls Risk, and High-Risk Maternity. The programs are categorized as Disease Management, Case Management, or Health and Wellness programs.
- Care plan
- Specifies the name of the clinical condition or chronic disease program that is being managed such as Diabetes, Asthma, Smoking Cessation, Post-Discharge or Re-Admission Prevention, Falls Risk, and High-Risk Maternity. The programs are categorized as Disease Management, Case Management, or Health and Wellness programs.
- Task
- Defines the automated and manual user actions such as scheduled phone calls, scheduled risk assessments, sending fulfillment, sending correspondence (emails and letters), and interventions.
- Goal
- Defines an objective to be met by the patient within a given time frame, for example, achieve HbA1c levels <7.
- Alert
- Defines the automated queries against claims and authorizations data sources that are used for monitoring changes, that is, the presence or absence of clinical events.
- Problem
- Defines issues that are associated with the patient that need to be addressed.
- Fulfillment
- Refers to documents, brochures, or educational materials that are sent to a patient or a patient's Primary Care Physician (PCP). By selecting this rule, you can attach these files to the associated program and program category.
- Barrier
- Defines situations that prevent a patient from completing a goal, including social determinants.
For more information, see the Diabetes example.
- Intervention
- Promotes behavior to improve mental and physical health or discourage or redirect those with health risks.
To create the components, see Creating your application components.
Program enrollment care plan
You create a care plan that includes a set of activities that are identified to manage the care of a patient. A care plan can contain problems, goals, barriers, tasks, and interventions.
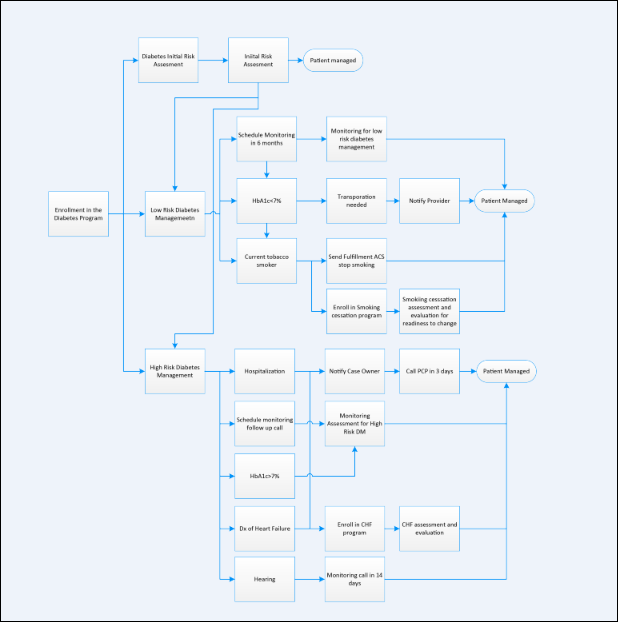
The following example shows that a patient is assessed for diabetes and then is enrolled into one of the three Diabetes Programs, based on the assessment.
- Initial Risk assessment
- This type of care plan is used to schedule an initial risk assessment task.
- Low Risk diabetes management
- This type of care plan is used to manage a low-risk diabetic.
- High Risk diabetes management
- This type of care plan is used to manage a high-risk diabetic with more active management.

Diabetes program example with three care plans
The following example shows that a Diabetes Program is managed with three care plans.
- Initial Risk Assessment Care Plan
- This type of care plan is used to schedule an initial risk assessment task.
- Low Risk DM Care Plan
- This example shows the types of alerts, goals, and tasks that can be set up to manage a low-risk diabetic.
- High Risk DM Care Plan
- This example shows the types of alerts, goals, and tasks that can be set up to manage a high-risk diabetic with more active management.
Previous topic Creating your application components in the Business Analyst portal Next topic Uploading code sets to Pega Foundation for Healthcare
