Claim business edits
This module (SBE) is responsible for performing in-claim edits, i.e. edits that utilize information on the current claim along with any associated configuration or reference data.
Claim business edits event codes
| Event code | Name | Description |
| SBE-0001 | Timely filing | The difference between the claim submission date and the claim line service date exceeds the configured timely filing days. |
| SBE-0011 | PCP required | A PCP (primary care physician) is required to deliver at least one service billed on the claim but the member has no PCP in the system. |
| SBE-0012 | PCP not affiliated with BE | The PCP's (primary care physician) NPI (national provider identifier) is not affiliated with the billing entity TIN (tax identification number). |
| SBE-0013 | Ineligible rendering provider | The services billed on the claim line must be rendered by a PCP (primary care physician) but the rendering provider is not a PCP or the rendering provider is not the member's PCP and is not affiliated to the same billing entity as the member's PCP. |
Timely filing edit
Timely filing requires that a provider submit a claim as soon as possible after the healthcare service has been provided. Typically, this can be for a year, but there can be different policies for different member contracts or states. The timely filing edit lets you configure the values associated with setting the timely filing event code and the sequence in which to apply it.
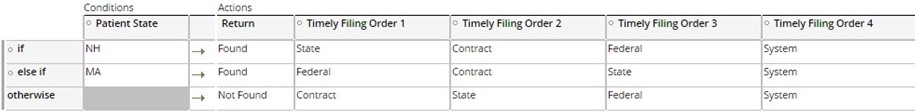
The timely filing value is configured in days and is used from a defined order of precedence. The delivered order is:
- Contract
- State
- Federal
- System (Default)
You can modify this order of precedence as necessary and you can configure each level in this order individually.
Each level in the order contains an optional value that represents the number of days to be used for that level to determine if the claim was received in a timely manner. The SCE starts at the top and continues through the order until it locates an available value. If no values have been found at the end of the order, the edit ultimately uses the system default timely filing settings.
The number of days retrieved by this method is subtracted from the service start date on the claim to determine the timely filing date. If the claim received date is after the calculated timely filing date, event code SBE-0001 is reported.
To configure the timely filing order edit, perform the following steps:
- Configure the order of precedence based on the state of the matched patient in
the CE_TimelyFilingStateOrder decision table
- Set the source and value of the edit to the appropriate value:
- For the Contract level, set the days value from the timely filing days setting in the Members Contract record
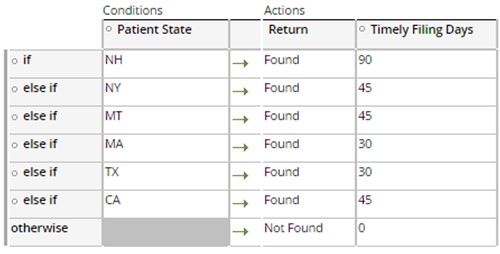
- For the State level, set the days value from the Patients state in the
TF_StateList decision table
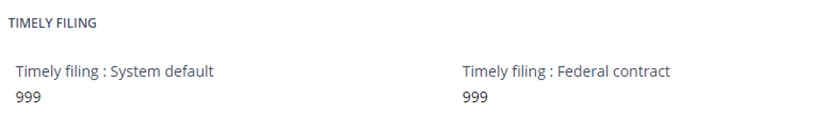
- The System default, and the Federal contract timely filing settings may be
configured in the Timely Filing section of the System Configuration page.
Note: the system default is a required property.
Validating primary care and unaffiliated providers
The Smart Claims Engine has the capability to match certain “unsolicited” providers (those who would not typically be eligible to bill) during claims adjudication when the benefit requires that the Primary Care Practitioner (PCP) be the rendering provider. The SCE allows for the delivery of a “PCP-only” service to a member by another provider as long as that provider is affiliated to the same Business entity as the member’s PCP, and is configured as a PCP under that Business entity’s TIN.
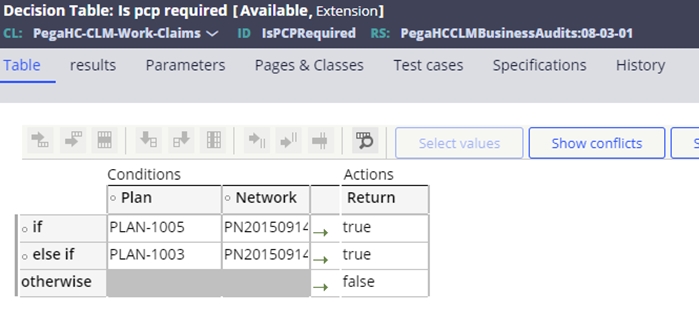
The configuration for the PCP requirement is the existence of the PCP required flag on the benefit. In the absence of this, the SCE also utilizes an IsPCPRequired decision table that can be configured to identify Plans and Networks requiring a PCP. The configuration of a discrete plan and/or network will determine whether all services included in the benefit require delivery exclusively by the member’s PCP.
If the PCP required flag is True, then the following edits will set:
- SBE-0011 – If the member does not have a PCP defined in the member record
- SBE-0012 – If the rendering provider is not affiliated to the PCP’s business entity
- SBE-0013 - If the rendering provider is affiliated to the PCP’s business entity, but is not configured as a PCP (covering practitioner) in its association to the business entity
Dynamic event codes
Dynamic events are executed during the processing of the Claim business edits module. The configuration for these event codes is documented in the section on event code configuration.
Previous topic Claim business rules and edits Next topic Claim business audits
