Claims information
The Claims UX has some primary sections that are detailed below. The fields on these screens may differ slightly between claim types and if the data was received or added during processing. The right sections on the UX are always displayed. Breadcrumbs are available when a link places the requested information in the primary section. These breadcrumbs will take you back to the previous screen.
The sections below detail the types of information that is held within each core section. The list of all fields on the claims UX is detailed in the Field labels section.
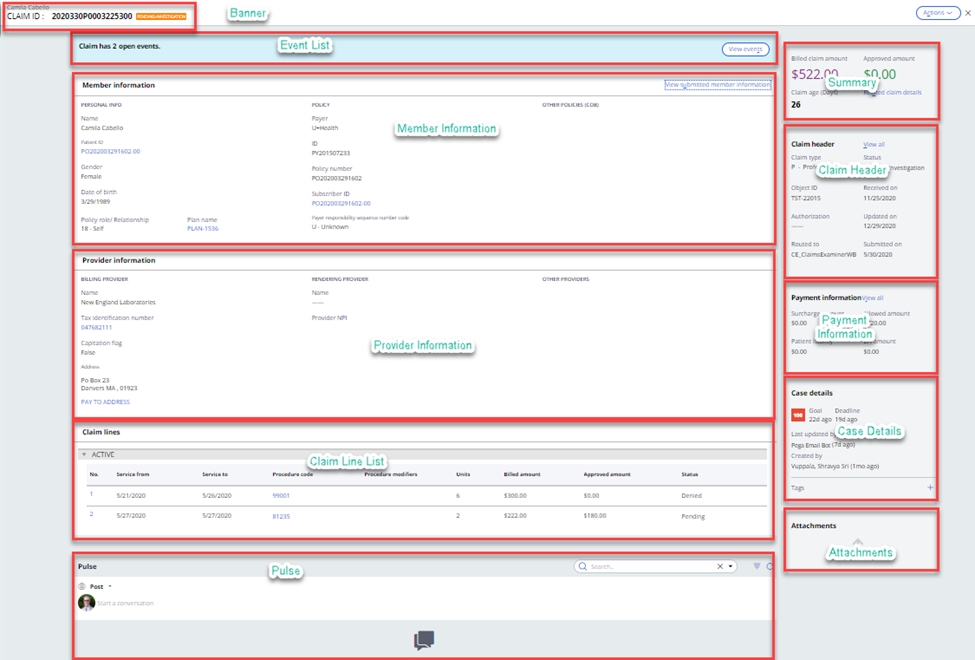
The claim banner contains the claim ICN (internal control number), the patient name and the status of the claim.
Event listIn the instance that the claim is still pending in the system and has open event codes associated with it, these are displayed here.
Member information sectionThe member section provides key information surrounding the member, patient and subscriber on the claim. Once the patient or subscriber has been matched to the member, then the matched information is displayed. A link to the original submitted information is provided.
The member information section on the UX is shown below. More information on the Patient, Subscriber, Plan or COB Payers can be found by selecting the hyperlinks.
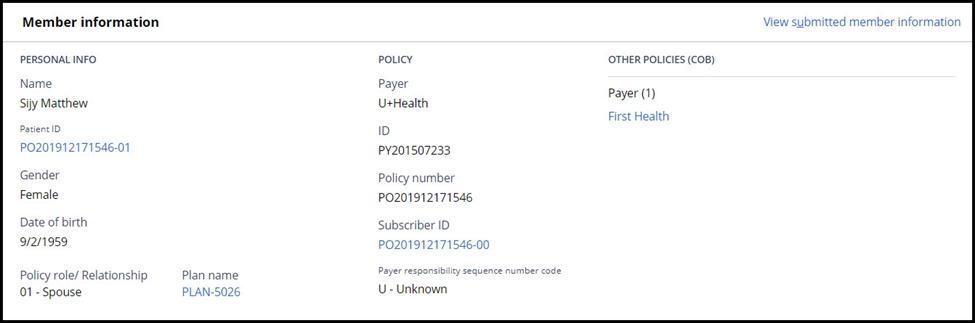
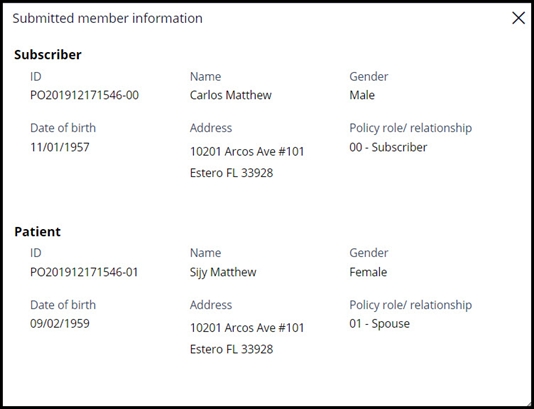
The information submitted on the claim for the patient and/or subscriber can be found by selecting the View submitted member information hyperlink. This will then display the original information submitted on the claim.
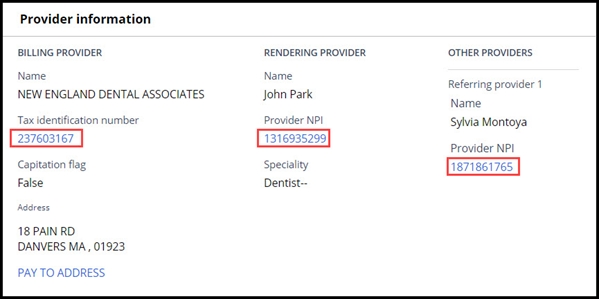
The provider section details key information about the providers submitted at the header of the claim. Provider information submitted at the line are displayed there. When the submitted providers are matched to providers in the system, hyperlinks are created to show more comprehensive provider information from the source system.
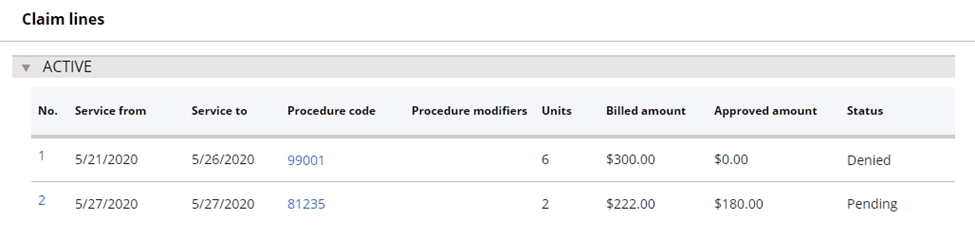
Claim lines are seen in the list, along with key information. Selecting the claim line will open the claim line details screen which contains more information about the line.
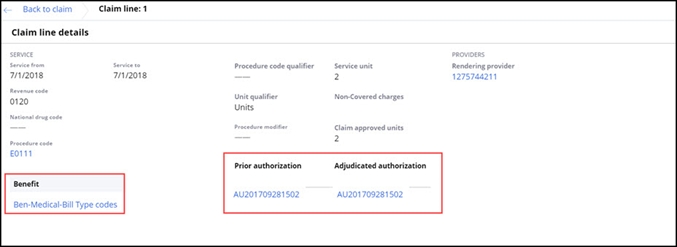
The claim line details screen provides access to information that was submitted or adjudicated on each of the claim lines. Access to more information, for example, the matched benefit, authorization or provider information is available via the hyperlinks.
The pulse section provides access to add or view any comments associated with the claim.
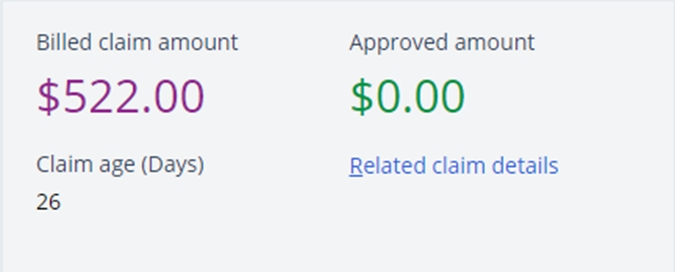
Claim summaryThe claim summary section provides key information on the claim that needs to be permanently displayed. In the instance that this claim is related to others, then the related claims link also appears in this section.
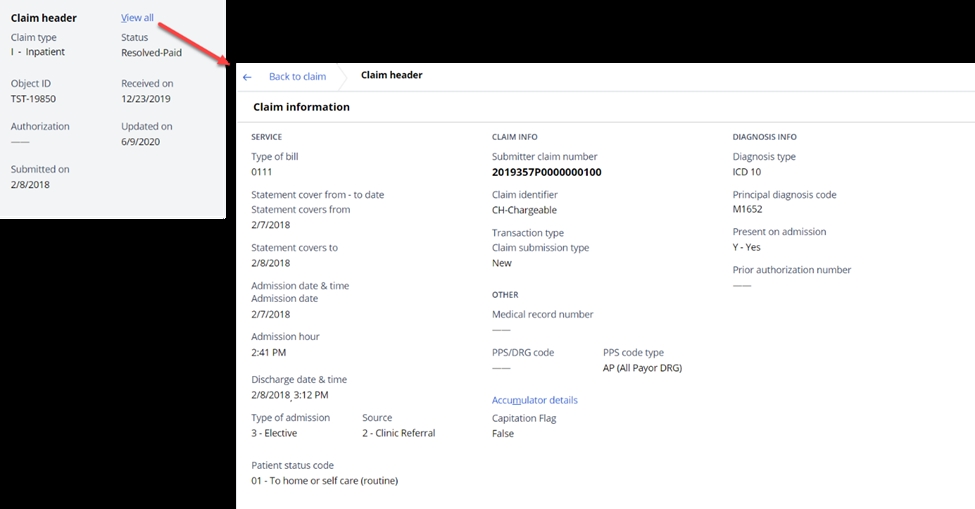
The claim header section provides a high-level summary of the claim header and the link to open the full set of details.
The Accumulator details hyperlink is displayed when any accumulator impacts the claim; selecting the link displays all the accumulators impacted by the claim and provides drill down access to further information.
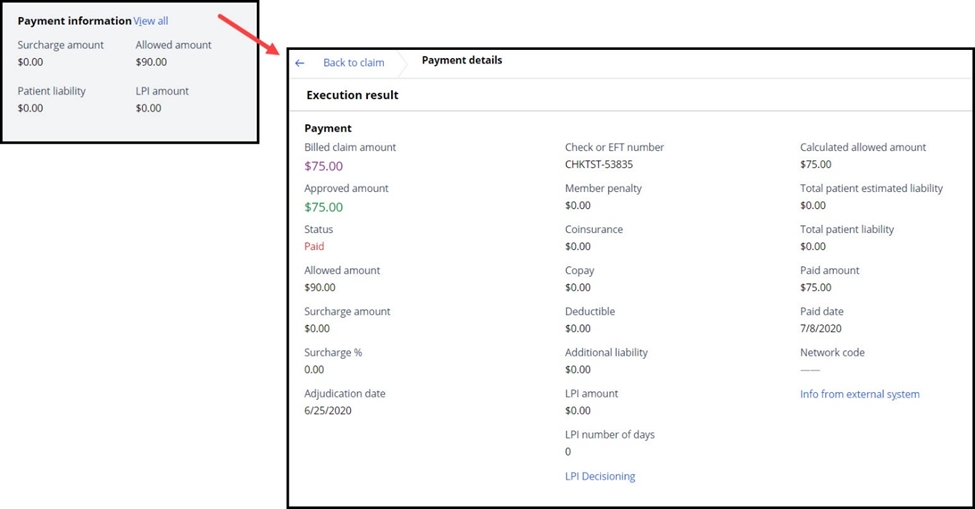
The payment section provides the high-level payment information on the claim, with the link to see the more detailed payment details and financial calculations.
The case details section shows key information about the claim case. These fields include the deadline and goal, the last update and any related tags that have been added.
AttachmentsThis section lists the attachments to the claim. Examples of these may include images from a scanned paper claim.
Key action menu itemsDetails on the full set of options available on the Actions menu are contained in the Claims Operations section.
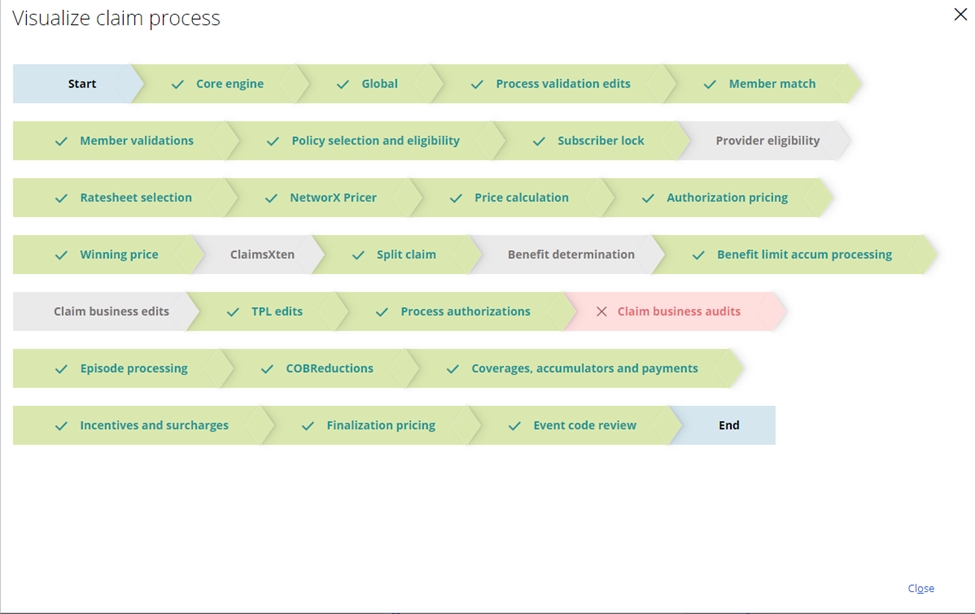
Visualize claim processThe SCE provides a graphical representation of the modules that have been executed during the most recent processing of a claim in the visualize claim process screen. Chevrons colored in green indicate a successful process, chevrons colored in red show that an open edit or error exists, and chevrons colored in grey show that the module was skipped. Clicking on each module will detail the process information for that module.
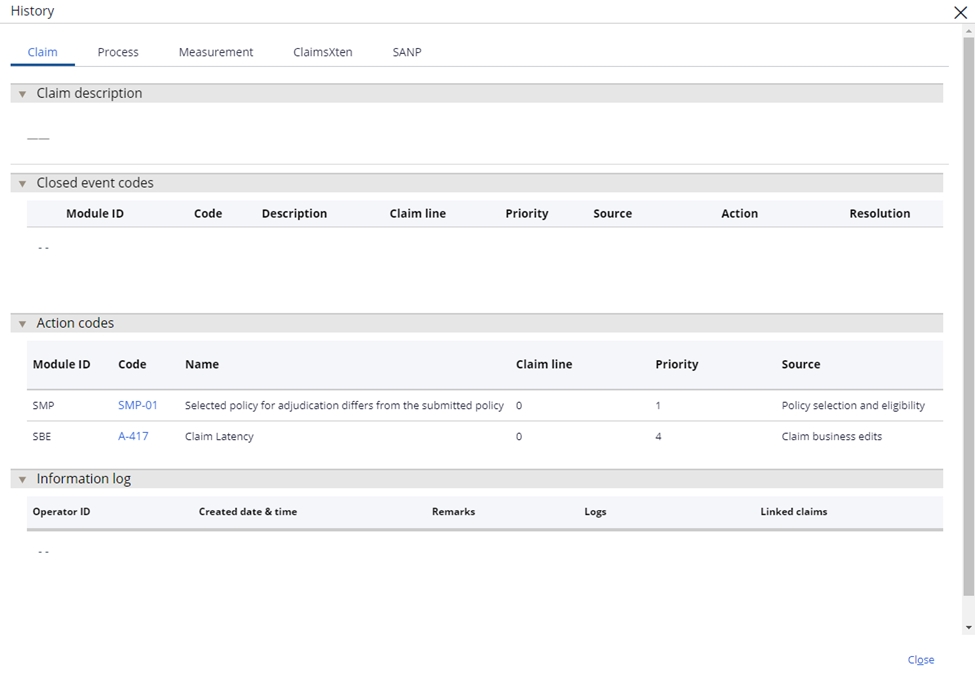
The SCE provides easy access to the audit trail and processing history for the claim. This is accessed through the view claim history option on the Actions menu. In this screen, the user can see detailed processing information, module timing and a summary of key actions on the claim. The claim tab (below) shows the key actions on the claim, including closed event codes, action codes that have been applied and any changes that an operator has made.
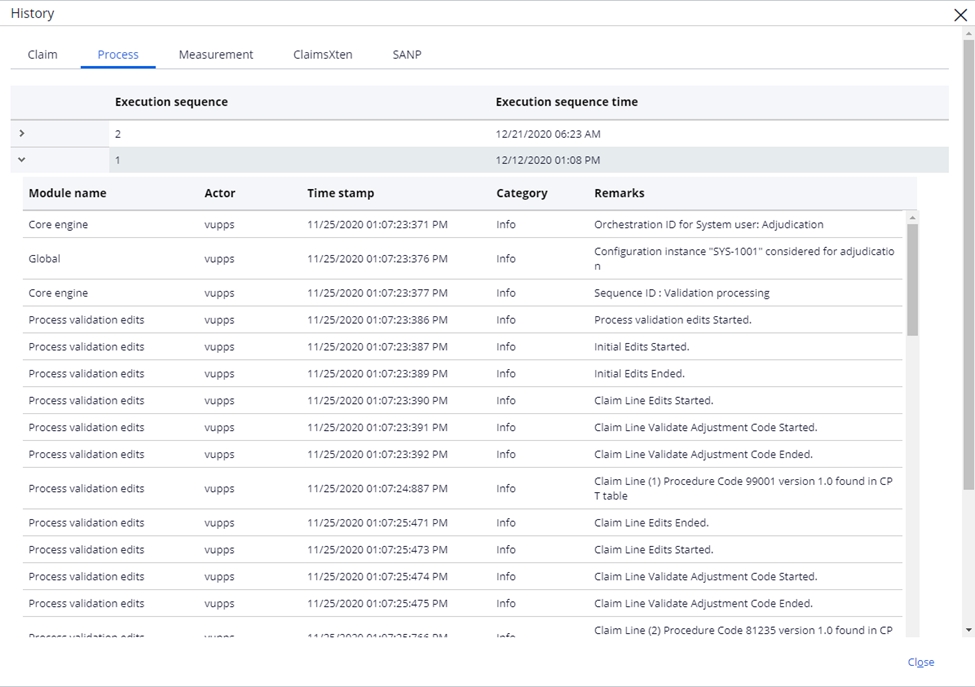
The process tab (below) shows the processing history on the claim for each execution sequence. This includes key information logged to the audit history by each module during the processing.
The measurement tab (below) shows the processing measurements on the claim for each module and execution sequence. This can show areas where processing time is exceeding expectations and SLAs.
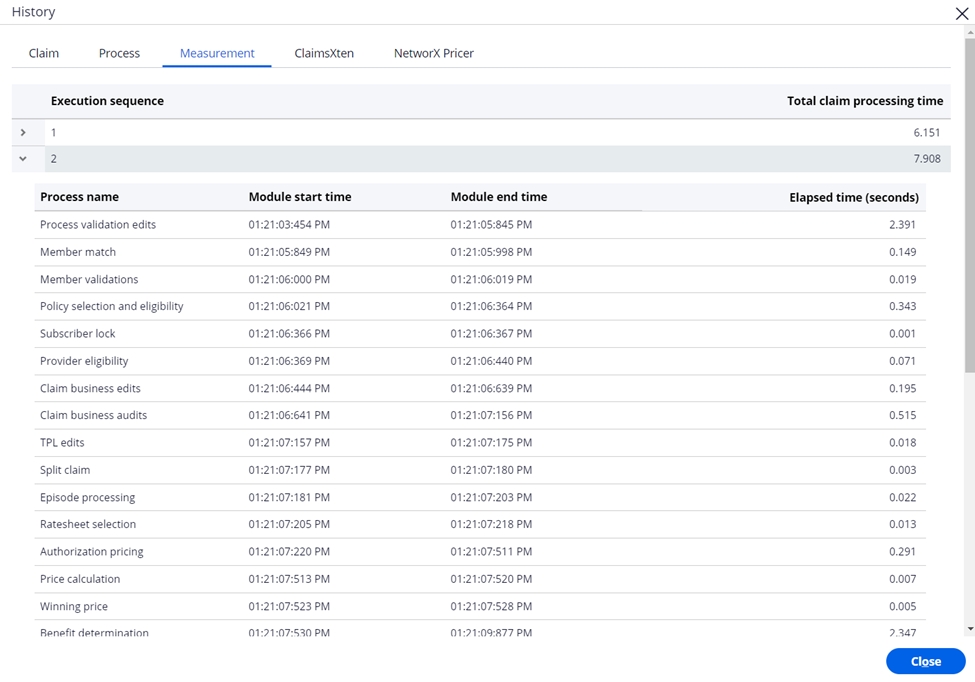
Information on the SANP and ClaimsXten tabs can be found in the sections on ClaimsXten and NetworX Pricer in the user guide.
View claim skills
The view claims skills item on the menu enables the claims examiner to review the skills that have been assigned to the claim during processing.
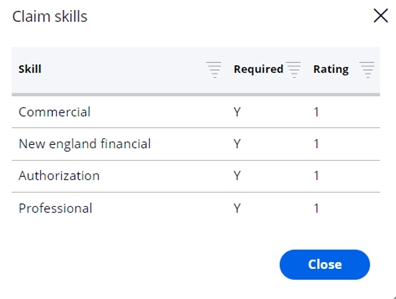
Note that this is only visible when the Bypass module setting for the skills assignment module (SSA) is Off.
Previous topic Key portal layouts Next topic Field level security
