Fraud and abuse edits
Smart Claims Engine for Healthcare provides comprehensive analysis and editing methodologies to protect the integrity of health plans as well as members, providers, and employer groups from fraudulent claims activities.
To detect Fraud and Abuse on the claim, Smart Claims Engine for Healthcare analyzes any practice on the claim that is not consistent with the goals of providing patients with services that are medically necessary, meet professionally recognized standards, and priced fairly.
Examples of medical or clinical abuse include billing for services that were not medically necessary, charging excessively for services or supplies, and misusing codes on a claim, such as upcoding or unbundling codes.
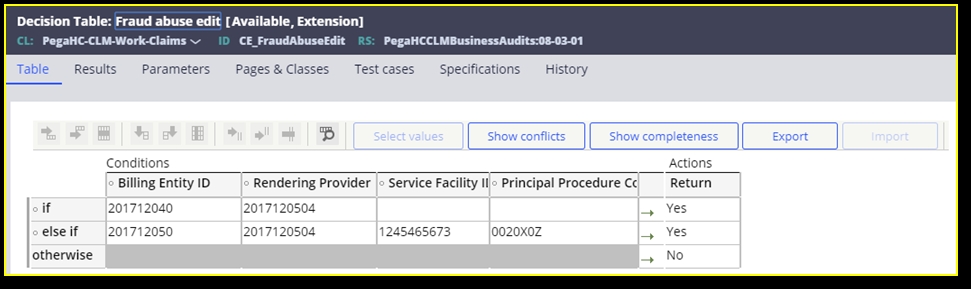
The Fraud and Abuse pend is configured in the CE_FraudAbuseEdit decision table used to hold billing entity ID, the rendering provider IDs, and procedure codes. If a claim matches all the values, then the fraud and abuse event code is set.
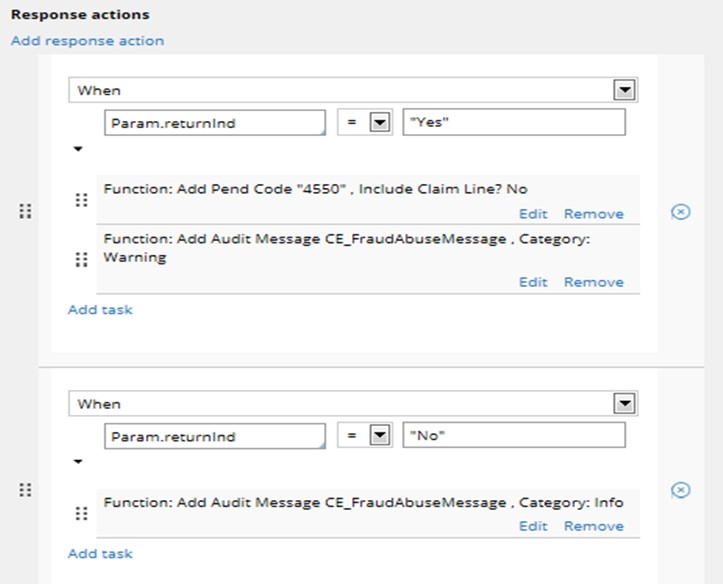
The following shows the claim engine configuration to process Fraud and Abuse edit.
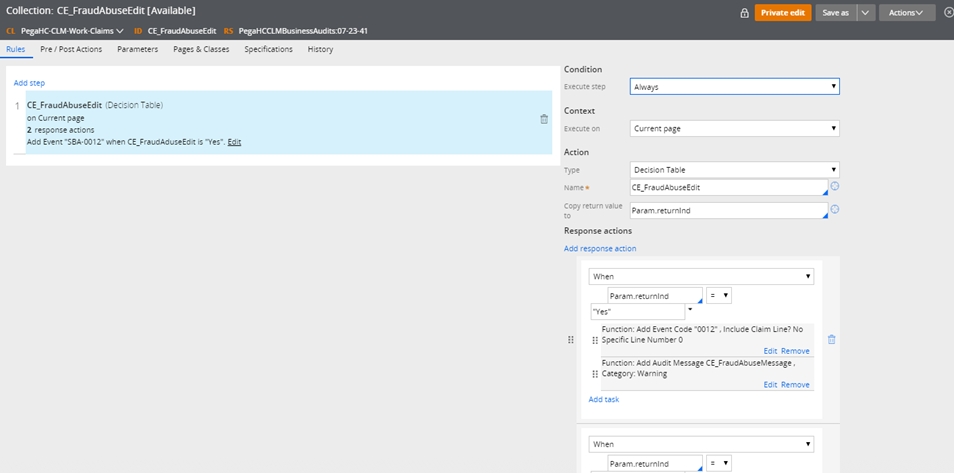
The Fraud and Abuse pend is configured in the CE_FraudAbuseEdit decision table used to hold billing entity ID, the rendering provider ID, service facility ID, and procedure code. If a claim matches all the values, then the fraud and abuse event code is set.
Currently, Smart Claims Engine for Healthcare sets one pend for Fraud and Abuse claim edit when possible fraud and abuse charges or practices are detected on the claim: Possible fraud and Abuse Edit – Event Code SBA-0012.
Previous topic D_CE_PatientHistoryDetails – Data Page Next topic Interim bill edits
