Claims business audits
Introduction
Claims business audits reveal discrepancies such as covering services not provided, paying for service not performed, and circumventing referral requirements. They discover duplicate payments, examine and analyze areas of possible fraud and abuse, and identify the inconsistency of the interim bills process.
This chapter is split into sections defining each of the audits that have been implemented.
Overview
The configuration of the Claim Business Audits is in the ProcessBusinessAudits collection rules under the application configuration.
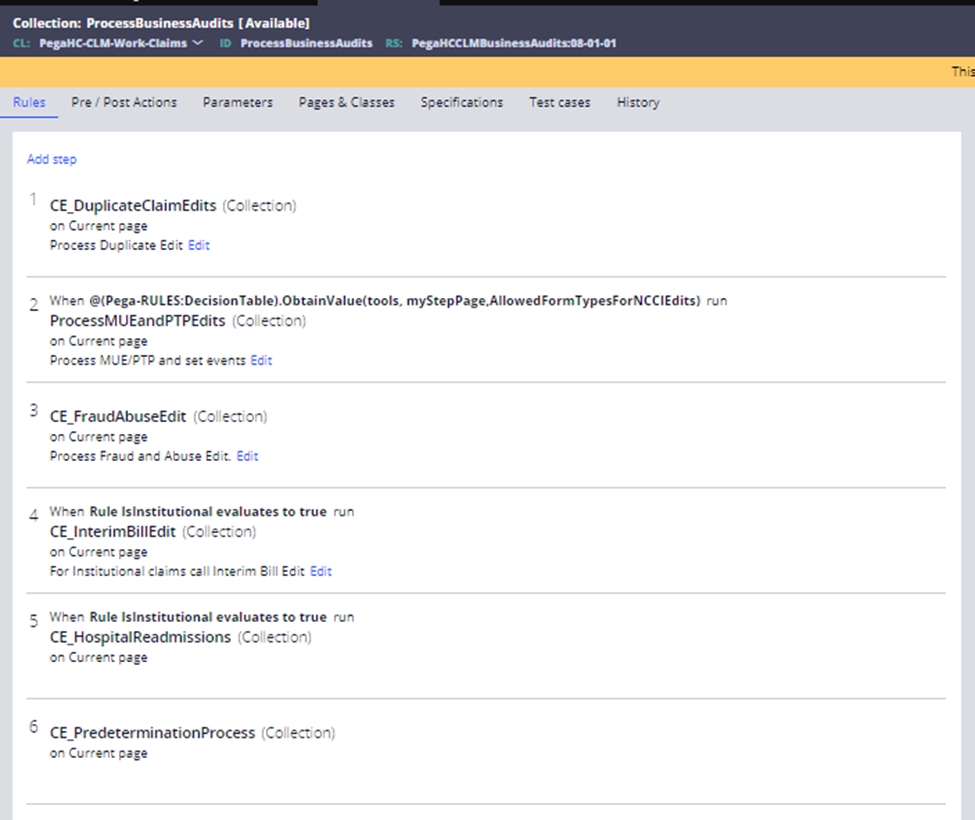
The ProcessBusinessAudits collection rule currently processes five types of claim adjudication edit:
- Duplicate Claim Edits – Supports exact and suspect duplicate claim pends.
- MUE and PTP Edits – Supports the editing of the claims with respect to the National Correct Coding Initiative (NCCI) with support for Medically Unlikely Edits (MUE) and Procedure to Procedure Edits (PTP).
- Fraud and Abuse Edits – Supports the infrastructure for defining fraud and abuse parameters.
- Interim Bill Edits – Supports the infrastructure for defining interim bill parameters.
- Hospital Readmission Audits – Supports the review of inpatient hospital claims, and the identification and resolution of unplanned hospital readmissions, according to the user’s business rules.
- Dental predetermination – Supports to adjudicate the Dental predetermination claim in SCE and also validating and searching the predeterminations for Billable claims
The core configuration of the Duplicate, Fraud, and Interim claim edits is on the Claim Edits Configuration screen. The Claim Edits configuration is used to validate incoming claims for processing. This function allows you to control claims processing by this application.
Previous topic Dynamic event check Next topic Duplicate claim edits
